As a small skeleton girl with a pear-shaped body, I grew up with slender upper limbs, a flat lower abdomen and thick thighs. One day three years ago, when I bowed my head, I stumbled upon that my lower abdomen had become round and round. The first reaction was “I’m getting older”, and the location of fat distribution began to change. So I started exercising regularly and also developed the habit of eating light meals.

Stomach bulges like air
For the next three years or so, although my weight remained stable, my belly continued to swell. Until this year, my entire abdomen and side waist were bulging like air, and it felt hard to the touch. While there were no other symptoms other than that, the exaggerated swelling made me realize I might be sick, so I decided to see a doctor.
The doctor prescribed a color Doppler ultrasound and the result was an ovarian cyst . Because my cyst is too huge, the color Doppler ultrasound can’t even give specific data. From the report, the “giant cystic mass” has occupied a considerable space in my abdominal cavity , and “up to the xiphoid process”, the entire uterus was also Completely blocked and not visible at all during inspection.
After seeing the results of the color Doppler ultrasound, the doctor advised me to be admitted to the hospital immediately and operated as soon as possible. In order to allow me to be hospitalized as soon as possible, the doctor did a gynecological examination and some preoperative sampling tests on me in the outpatient clinic.
I have no previous experience with a gynecologist, and this is the first time I’ve been on an exam bed. At first I only had a slight fear, more of the calmness of “the fearless of the ignorant”, but when the instrument penetrated into the body, my body tightened instantly, and I cried out in uncontrollable pain. After several unsuccessful attempts, the doctor had to let me rest for a while and then resample.
After admission, doctors further arranged for an MRI. During the examination, the doctor adjusted my position while scanning, but even as I was moved around in the cabin, I couldn’t see all the edges and details of the cyst. On the MRI film, my entire abdominal and pelvic cavity was filled with cysts, and all the adjacent organs were squeezed around . Compared with the cysts, these organs appeared small.

MRI image丨Photo courtesy of the author

After pumping fluid and cutting the cyst, I lost 12 pounds after the operation.
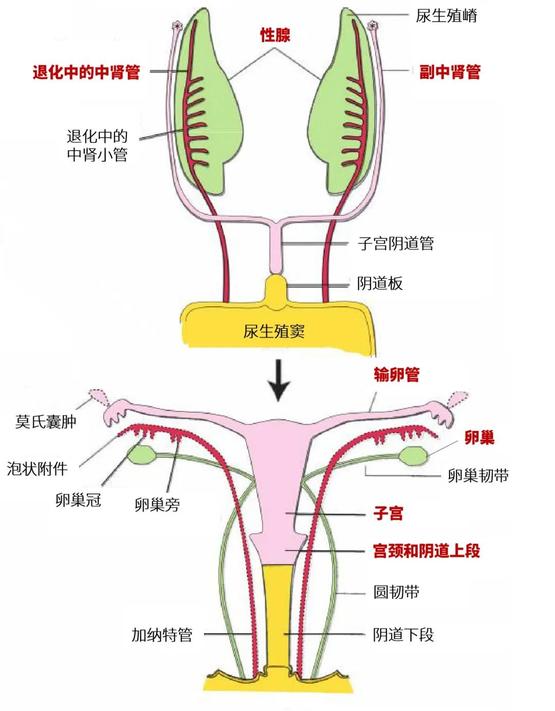
Immediately after admission, I had surgery. The doctor told me after the operation that all the cysts were removed, and the largest cyst was about 25×20×20cm. Intraoperative quick frozen section showed mature cystic teratoma and paramesonephric duct cyst, both benign. The doctor removed about 3500ml of fluid from my cyst. Immediately after the operation, I lost 12 pounds, and my weight dropped from 98 pounds to 86 pounds, which is a number I have never seen since my height stabilized.
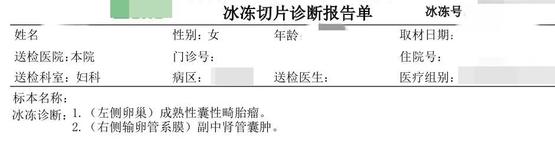
Intraoperative rapid freezing report丨Photo provided by the author
The doctor explained that it is necessary to move as much as possible after the operation to avoid thrombosis due to lying down for too long; the diet should also be gradual from liquid food to normal diet, otherwise the digestive system will be prone to problems. The doctor also warned me that because I am relatively thin, with thin sebum layer and weak skin tension, there is a risk of surgical incisional hernia at the wound in the future.
What happened to me, however, was another complication of laparoscopic surgery, which I’ll call “bleeding.” The surgery I did was a single hole laparoscope, and only one hole was punched at the belly button. Laparoscopic surgery is also porous, but no matter the single orifice is porous, the gas that is harmless to the body will be injected into the abdominal cavity, so that the abdominal cavity can be swelled so that surgical operations can be performed in this swelled space. Although gas will be released at the end of the operation, there is still the possibility of gas remaining, which needs to be absorbed and discharged slowly.

To take out the huge cyst, only a belly button-sized hole is needed.丨Photo courtesy of the author
The patients who underwent surgery at the same time as me were basically not troubled by “channeling gas”, but my road to “channeling gas” was very difficult. I could barely get out of bed three days after the operation, and the “channeling gas” did not completely disappear for a month after the operation.
The pain of “channeling gas” can only be understood by those who have experienced it. Can’t get up, can’t turn over, can’t move his legs casually, and his body can almost only be fixed on the bed. If I was a little careless, a burst of air would instantly press against my chest and throat, so I was so sore that I couldn’t speak or even breathe. The only way to relieve it was to lie down immediately.
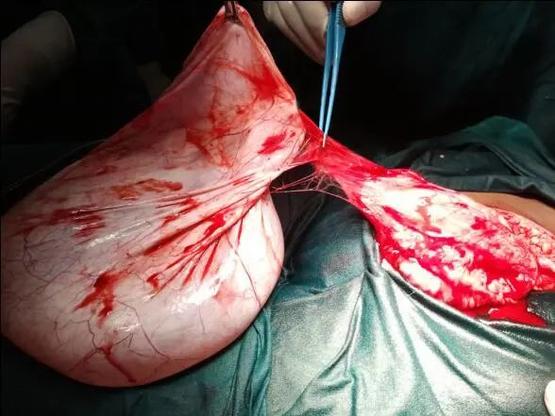
Alas, the surgery is not easy. A few days after the operation, the final pathological examination came out. There were mature cystic teratoma in the left and right ovaries, and a paramesonephric duct cyst in the right mesosalpinx .
Postoperative pathological examination diagram丨Photo courtesy of the author
This experience has made me understand that physical problems must not be taken lightly. We must develop the habit of regular physical examinations, and seek medical attention in time if you feel unwell.
At the same time, do not have any prejudice and stigma against gynecological diseases. During the consultation process, many people wondered that I had gynecological diseases in my twenties, but this was actually prejudice and discrimination. Women do not suddenly develop a female reproductive system when they become adults, let alone after marriage. This is the body we are born with.
Doctor Reviews
Liang Tingting | Deputy Chief Physician, Department of Obstetrics and Gynecology, Second Hospital of Shanxi Medical University
The composition of ovarian tissue is very complex, and it is the organ with the largest number of primary tumor types in various organs of the body. point.
In Nutshell patients, we have already known some types of ovarian tumors. We will not repeat the mature teratoma here. Paramesonephric cyst.
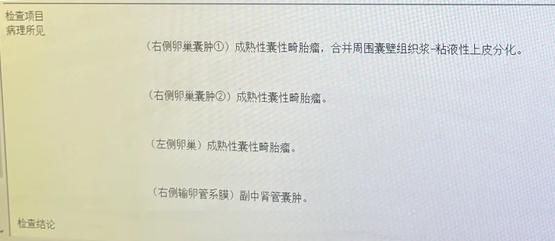
Let us first introduce what is the accessory mesonephric duct. In the embryonic period, before the gonads are not differentiated into male gonads and female gonads, regardless of gender, there are two longitudinal pairs of primitive ducts in the embryo, namely the mesonephric duct (Wolffian duct) and the paramesonephric duct (Müllerian duct, Also known as the mesonephric paratubule), and gradually descends from the original kidney to the pelvic cavity.
After 6 weeks of embryonic, primitive gonads begin to differentiate. If there is a Y chromosome, the gonads differentiate towards the testes. At the 8th week of the embryo, the formed Sertoli cells secrete paramesonephric inhibitory factor (MIF), which degenerates the paramesonephric duct; at the same time, MIF stimulates Leydig cells to secrete testosterone, which differentiates the mesonephric duct into male internal genitalia. Including the vas deferens, epididymis, ejaculatory ducts and seminal vesicles.
In female fetuses without a Y chromosome, the gonads gradually differentiate and develop into ovaries. Because there is no testis to secrete MIF, the accessory mesonephric duct does not degenerate, but gradually develops into the female internal genitalia, including the fallopian tube, uterus and upper vagina from top to bottom ; at the same time, because there is no stimulation of MIF, the mesonephric duct degenerates.
Schematic diagram of the evolution of the female reproductive system. The accessory mesonephric ducts marked in pink gradually evolve into fallopian tubes, uterus and upper vagina, and the mesonephric ducts marked in red gradually degenerate.丨Reference 2
Paramesonephric Cysts (PMCs) are non-neoplastic cysts that can occur in both men and women. It is derived from the embryonic residue, and the thin layer of epithelium on the inner wall of the cyst will secrete a large amount of cyst fluid to expand the cyst. PMCs are mostly benign, and borderline or malignant paramesonephric-derived tumors are extremely rare.
In women, PMCs mostly occur in the broad ligament between the ovary and the uterus, next to the ovary, or on the mesosalpinx . In addition, there are also case reports of occurrence in the vagina, groin, etc.
The size of PMCs varies, and the giant PMCs mostly occur in the broad ligament. There is a clinical case of a 25-year-old female with bilateral paraovarian giant PMCs (40×40cm, 30×30cm). Patients are generally asymptomatic. When the cyst is large, compression symptoms, such as abdominal distention and abdominal pain, may occur . Common complications include bleeding, perforation, and torsion. When the diameter of the cyst is greater than 5 cm, the risk of torsion is greater.

A 40×40cm paramesonephric duct cyst seen during surgery丨Reference 3
Before surgery, it is difficult to distinguish PMCs from other types of benign and malignant tumors, and it mainly relies on imaging examinations such as ultrasound, nuclear magnetic resonance, CT, and tumor markers. When imaging studies reveal papillary protrusions within the cyst, it suggests an increased risk of malignancy.
The resection of PMCs depends on surgery, and laparoscopic or open surgery can be selected . It needs to be comprehensively considered according to the operator’s operating level, whether malignant tumors are suspected, and the patient’s tolerance to surgery. The diagnosis of PMCs also depends on postoperative pathological examination , which needs to be differentiated from mesonephric cysts under the microscope.
Where there are organs there is the potential for disease, as is the reproductive system. The pelvic cavity is deep and low, and it is not easy to detect the tumor as early as possible. As the author said, it is necessary to have the habit of regular physical examination, and to seek medical treatment in time if there are symptoms of discomfort, so as to detect lesions at an early stage.
references
[1] Zhang Lei, Cui Yueqiang. Clinical and imaging analysis of paramesonephric duct cyst in female reproductive system [J]. Journal of Clinical Radiology, 2020, 39(09): 1812-1815. DOI: 10.13437 /j.cnki.jcr. 2020.09.030.
[2] Ronald W. Dudek. BRS Embryology 6th edition. 2014.
[3]Sagili H, Krishnan M, Dasari P. Huge Bilateral Paramesonephric Cysts in a 25 year old Nulliparous woman. J Clin Diagn Res. 2013 Nov;7(11):2589-90. doi: 10.7860 /JCDR/2013/6563.3597 . Epub 2013 Nov 10. PMID: 24392412; PMCID: PMC3879885.
Personal experience sharing does not constitute diagnosis and treatment advice, and cannot replace a doctor’s individual judgment on a specific patient. If you need to seek medical treatment, please go to a regular hospital.
Author: ee
Editor: Xiao Ai, Li Xiaoqiu
Here is the Nutshell patient, focused on telling health stories.
If you have an experience of getting sick or seeing a doctor to share, or want to talk about your own health-related anecdotes, please submit your articles to [email protected]

This article is from the guokr patient (ID: health_guokr), and may not be reproduced without authorization. If necessary, please contact [email protected]
This article is reproduced from: http://www.guokr.com/article/462788/
This site is for inclusion only, and the copyright belongs to the original author.