This story is partly adapted from “Care: A Decade of a Harvard Physician and Wife with Alzheimer’s Disease.” Today is the 29th “World Alzheimer’s Disease Day”, and this year’s theme is “Know yourself, know the enemy, prevent early wisdom and join hands to the future”. As Alzheimer’s disease progresses, patients will gradually lose their ability to take care of themselves, and caregiving will become a huge challenge, putting the physical and mental health of caregivers at risk . Understanding and caring for caregivers is the hope for the entire family to move forward.
“Get out!” My wife woke up from her nap to find a strange man lying on the bed. She was terrified, screaming and beating him like crazy.
But that “stranger man” was none other than me, the husband who had been with her for more than 40 years. I’m a trained psychiatrist, and I’m teaching patient care in medical school, so I should be able to handle it all. But at the moment it happened, I was still a terrified and heartbroken husband.
However, it is not the most hopeless that my wife does not recognize me. After she was diagnosed with Alzheimer’s disease, the inability to take care of her for a while, her more frequent tantrums, and her refusal to dress and eat make me feel tired and frustrated. , even angry.
It’s my wife who’s sick and I’m her primary caregiver, but now it’s me who needs help more urgently.

Care work besieged me | pixabay
tired and depressed
But how can I selfishly escape the care of my lover?
His wife used to be a university professor, but when she was in her fifties, she gradually couldn’t read the news and couldn’t calculate the price. I took her to the best neurologist and got the most advanced tests and medications at the time, but out of the hospital, most of the care fell to my family, mainly me:
Every morning at six o’clock, I wake my wife up, take her to the bathroom, hand her toilet paper and wash my hands. Then I help her put on her sweatpants and take her out for a walk. When I got home, I helped her to take a shower and change her clothes. After that, I would lead my wife to the kitchen to sit down, prepare breakfast, and feed her slowly.
After dinner, I took my wife to the office to watch her while she was working so she wouldn’t hurt herself at home alone.
After get off work, I go home to cook, feed, watch TV and explain the news to her. At night, I put her pajamas on, brush her teeth, and get ready for bed. During this period, I have to keep answering her questions, such as repeating dozens of times about what I did today.
If all goes well, my wife will soon fall asleep, I quietly get up, close the door, wash the dishes, tidy up the room, prepare food and medicine for the next day, and prepare for work. When I finally got back to bed, I ran through my mind what I was going to do for the next 12 hours: get her up at night to go to the bathroom, so she wouldn’t soil the bed and floor again with incontinence; get up early so I had enough time to be calm and gentle Help her bathe and dress; and finally, hope that my wife doesn’t wake up in the middle of the night yelling, walking around the house, or punching and kicking me.

Wake up the next day and I’ll repeat it all | pixabay
Despite being tired, I’ve grown accustomed to taking care of my wife like this. But at the last family reunion, my wife didn’t want to talk to everyone, she looked frustrated and scared, and my son got mad at me because of it. He felt that she gave so much to my career and my whole family when she was young, and now I’m selfish, failed to take care of her. I got into an argument with my son, then broke down and wept, causing everyone to cry.
It dawned on me that I had been doing almost all of my caregiving alone because I felt it was my sole responsibility. Now, ten hours a day of nursing care makes me very tired, and the results of my medical examination are not as good as before. I still don’t want my wife to miss parties and walks, to eat a makeshift meal, to wear diapers, and to interrupt impatiently. Her repeated questions… I couldn’t do everything I wanted to do, fell into self-blame and powerlessness, and became easily irritated.
A change had to be made, and I needed to ensure my own health, the help of my children and family and friends, and the time to breathe.
I was very fortunate to have found a caring and tolerant home care worker who was responsible for the daytime care. After my wife accepted the carer, I was finally able to work with peace of mind. More importantly, I was less worried and anxious while taking care of my wife , my uncontrollable temper became better, and my wife felt less guilt about my care , and the shaky relationship between the two at the time stabilized.
Once, I could not imagine putting my lover in the care of others, but without the help of the nurse, I might have collapsed and it would be difficult to continue to take care of my wife at home, so I could only choose to give up completely.
How to reduce caregiving stress
“Caring” means helping those in need (such as young, elderly or sick relatives), even the strongest of people who can still suffer both physical and psychological pain in the process of caring for a loved one . Alzheimer’s disease is more stressful for caregivers than other chronic diseases.
Significant recent weight gain or loss, lack of sleep, body aches, easy anger, feeling tired or sad, loss of interest in things you used to enjoy are all signs of too much stress.
1. Protect your caring capacity: Instead of having to do everything alone, let professionals, family and friends share responsibilities, such as spending short time with them, helping with shopping or cooking. Don’t feel guilty about taking time to do your own thing, taking a break and getting away is a good thing for both the caregiver and the care recipient.
2. “Imperfect” is inevitable: Even with good care, many progressive diseases continue to worsen. Learn about the disease, don’t try to do things beyond your ability, and believe that you have done your best and made the best decision.
3. Do the most important things first: Make a list and prioritize tasks, such as considering easy-to-prepare food, reducing the number of baths.
4. Take care of yourself before you can take care of others : try to maintain healthy sleep, diet and exercise habits, and seek help from relatives, friends and doctors when needed.
next level of hell
It’s my wife’s mania that ignites my anger
The caregiver eased our lives, I was able to relax for a while, and I saw a smile on my wife’s face more often.
But the disease not only silently erased the memory of how his wife lived and the traces of his family, but also raised anxiety and panic. I just felt like I was finally in control of my life, everything fell apart again, and we fell to the next level of hell again.
The wife’s mood became increasingly unstable and unpredictable, and she sometimes experienced hallucinations and delusions, such as suddenly speaking loudly into the air, or believing that her food was poisonous and that someone was trying to steal her belongings. This uncontrollable frenzy was the most powerless part of caring for her , and made taking her out of the house even more difficult:
One year for my wife’s birthday, we went to a fancy restaurant to celebrate, along with my mother, brother and sister-in-law. When we were seated, my wife jumped to her feet and yelled at me angrily that she was no longer a child and didn’t need me to help her sit on the chair. A few minutes later, she got up from her chair again, making a fuss because we didn’t order her wine. But in fact, she was not allowed to drink alcohol while on medication.
Soon, we alarmed everyone in the store. The whole dinner was like a prelude to a disaster, full of tension, and every few minutes the wife would lose her temper. When I finally left, I tried to pull her into the car, but she resisted so hard I had to rush into the hustle and bustle of traffic to pull her back into the car. On the way home, she threatened to jump out of the car door to end it all.
By the time we finally got home, my wife had become quite manic, knocking over a small table and throwing the paintings and other things on the wall onto the floor. At this point, I could hardly hold back the anger in my heart, and I wondered if I could endure it, and this was not the first time I had thought so.
The wife refused to change her clothes or go to bed, until she fell asleep on the sofa because of the irritable heat. I put a blanket over her and slumped in the chair for hours. I blamed myself for my anger and didn’t know what else to do.
By the next morning, she had no idea what had happened the night before: “Why are we sleeping in the living room?”
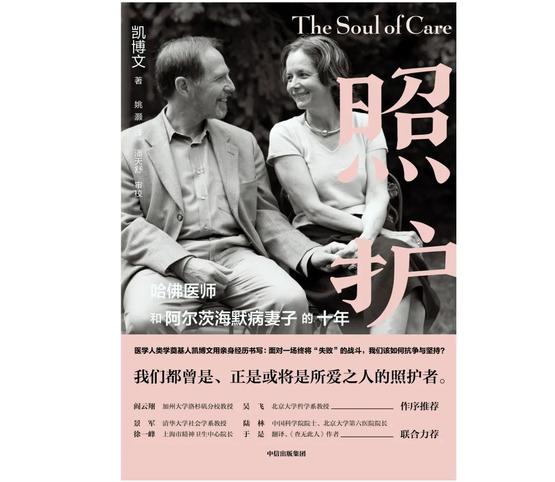
“Care: A Decade of a Harvard Physician and His Alzheimer’s Wife” | CITIC Press
Alzheimer’s disease is brutal, and for caregivers, one of the reasons it robs a critical part of the care process, the care recipient’s feedback.
Sometimes my wife responds warmly and gratefully to my care, grinning; other times she yells and resents me for imaginary reasons; By how I explain it, she just wouldn’t let me get close to her. The wife might get better in a few hours, and even laugh at what happened before. But my heart is broken and I feel like I’m getting nothing in return for what I’ve done.
I can explain from a medical point of view how the disease caused my wife’s behavior and emotions to be abnormal, but as someone who cared for her day and night, it was like the bond between us – the bond that has been forged over the past half century, It snapped in an instant.
When pain, resentment, and exhaustion begin to invade the caregiving relationship, it can turn into verbal, mental abuse, or even physical violence . Fortunately, my medical training made me alert to my mood swings and other warning signs, and I accepted my angry feelings without completely losing control.
How to deal with negative emotions
Alzheimer’s disease can cause patients to lose memories of loved ones and to be angry and dissatisfied with their caregivers. More than 80% of patients experienced neuropsychiatric symptoms, including apathy, irritability, depression, and delusions, which significantly increased caregiver stress.
It is normal for a caregiver to feel overwhelmed, angry, frustrated, exhausted, or sad, and it can also have negative feelings about the patient and caregiving responsibilities . This does not mean that you are an unqualified caregiver. After accepting your emotions, you can try the following ways to improve:
1. Get support from others: caring at home alone is easy to be isolated, and when the care recipient cannot express gratitude, often talk to family, friends and other caregivers for recognition and encouragement;
2. Remind yourself often: I’m doing my best, what I’m doing is hard for anyone , I’m not perfect but that’s okay, I’ll enjoy the moments when we can be at peace, the patient may be behaving abnormally because sickness, not what I do;
3. About 40% of Alzheimer’s disease caregivers have symptoms of anxiety and depression, and they need to seek help from mental and mental health professionals in time to protect the mental health of caregivers and avoid abuse of patients.
I promise to always take care of my wife at home
But finally betrayed her
There have been good and bad days, my heart has been broken and whole, and the tasks and suffering have not diminished, but we still have a little joy in the cramped world framed by this annoying disease.
Every day, I work on the small details that need to be solved urgently now, while putting aside the big issues like the entire Alzheimer’s care journey. I hadn’t thought about the final stages of my illness, but occasionally thought that if I left earlier than my wife, and my children had a life of their own and lived far away, I probably wouldn’t be able to take care of my wife at home or visit her often in a nursing home. The thought was so depressing that I was always trying desperately to suppress or deny it.
In my 10th year of care, there were a few very rough weeks, and despite taking several medications, the wife was still in a state of uncontrollable madness every two days.
One night, she smashed the painting on the wall and several dishes, shouted that I was a stranger and was going to hurt her, and then lay on the floor kicking and yelling. I tried to reassure her as gently as I could, but to no avail. I sat down so hard that I couldn’t even shed tears. It was as if there was an impenetrable wall standing in front of me, and I couldn’t see how I could move on, so I could only let despair engulf her.
After my wife fell asleep on the floor, I called a specialist in psychiatric medication for advanced dementia and he recommended that she be hospitalized immediately. I stayed up all night and sent my wife to the geriatric neuropsychiatric ward the next day . When I was home alone, I finally couldn’t hold back the tears when I called my children and felt like a failure.
Over the years, I’ve made taking care of my wife at home as the only option, and I’ve made a promise to her. But in the end, I couldn’t make it.
The family found a well-cared-for nursing home, and the wife was transferred after her condition stabilized . Over the next nine months, she gradually lost the ability to move her limbs and slept longer and longer. I go to see her every day, sometimes she recognizes me and smiles, but more often she just seems to be lost in the final journey of her life. During this time, I felt isolated and overwhelmed, even though my children and family came to visit me frequently.
My wife was fading, and my family and I respected her repeated pleas—no hold back. This plea has been formally recorded in her living will and power of attorney. The whole family sat around her bed, recalling many stories from the past, saying goodbye to her, until she left peacefully late one night.
Now that my wife has been away from me for 7 years, at least a part of that frustrating but helpful experience of caring has turned into my heart and evoked the love in my soul. In the process of reminiscing, my grief for her gradually turned into a treasure for myself.
Those 10 years of care taught me that it can’t be perfect: no matter how much we expect once and for all victory, how hard we plan and give, we are all trapped in vulnerable situations, and the process of care is full of exhaustion and failure, just as Dotted with hopes of balance and contentment.
Create a long-term care plan
Once the pattern of disease progression is understood, discussions can begin with family members as early as possible so that the patient can also participate in the decision-making process. Mutual agreement on long-term care at home or institution, when to change care, medical options, and even burial. Discuss legal and financial issues. Facing it early can better respect the patient’s wishes and help caregivers accept reality.
Primary caregivers should plan for their own unexpected situations, discuss alternative care methods and caregivers with relatives and friends, and leave the necessary information for the next caregiver : the patient’s illness and treatment, assistance needed in life, preferences and dislikes, existing behavioral problems, and how to help them calm down.
Even after care has ended, symptoms such as depression and anxiety can plague caregivers for years and require ongoing psychological support.
Of course, each story is played out in its own world. I know Alzheimer’s disease well, have close and strong relationships with family and friends, and have good financial and social resources that support my wife and I against the storm of disease and care.
There are still more than 50 million patients suffering from Alzheimer’s disease in the world. There are about 10 million patients over the age of 60 in China , and the prevalence rate of people over the age of 85 is nearly 50%. More than 90% of the patients are cared for by their families . Each caregiver faces unique physical and mental health conditions, family relationships, work and financial pressures, and customs, and therefore has different caring styles, processes and feelings, but all will experience stress and frustration , and need the support of those around you.
With Alzheimer’s disease, we’re still looking for ways to stop the disease from reaching its end, and family caregivers still carry the heaviest burden of care. Keeping the caregiver’s light on, the whole family can continue to support and move forward in the fog of suffering.
references
[1] Author: Kai Bowen, Translator: Yao Hao. 2020. Nursing: A Decade of a Harvard Physician and His Wife with Alzheimer’s Disease. CITIC Press.
[2] China Alzheimer’s Disease Report Writing Group. China Alzheimer’s Disease Report 2021. Diagnostic Theory and Practice. 2021;20(4):317-337.
[3] Iravani B, Abdollahi E, Eslamdoust-Siahestalkhi F, Soleimani R. Neuropsychiatric Symptoms of Alzheimer’s Disease and Caregiver Burden. Front Neurol. 2022;13:877143.
[4]Chen P, Guarino PD, Dysken MW, Pallaki M, Asthana S, Llorente MD, Love S, Vertrees JE, Schellenberg GD, Sano M. Neuropsychiatric Symptoms and Caregiver Burden in Individuals With Alzheimer’s Disease: The TEAM-AD VA Cooperative Study. J Geriatr Psychiatry Neurol. 2018;31(4):177-185.
[5] Terum TM, Andersen JR, Rongve A, Aarsland D, Svendsboe EJ, Testad I. The relationship of specific items on the Neuropsychiatric Inventory to caregiver burden in dementia: a systematic review. Int J Geriatr Psychiatry. 2017;32(7 ): 703-717.
[6] Corey KL, McCurry MK, Sethares KA, Bourbonniere M, Hirschman KB, Meghani SH. Predictors of psychological distress and sleep quality in former family caregivers of people with dementia. Aging Ment Health. 2020;24(2):233- 241.
[7]Magan KC, Hirschman KB, Starr LT, Meghani SH. Longitudinal Trajectories and Correlates of Post-Caregiving Depressive Symptoms in Former Caregivers of Persons With Alzheimer’s Disease or a Related Dementia. Am J Hosp Palliat Care. 2022;39(6) :725-736.
[8] Vu M, Mangal R, Stead T, Lopez-Ortiz C, Ganti L. Impact of Alzheimer’s Disease on Caregivers in the United States. Health Psychol Res. 2022;10(3):37454.
[9] Cox, C. Factors Associated with the Health and Well-being of Dementia Caregivers. Curr Tran Geriatr Gerontol Rep 2. 2013, 31–36.
[10]Susan D Gilster, PhD, RN, LNHA, Marie Boltz, PhD, GNP-BC, FGSA, FAAN, Jennifer L Dalessandro, BSHSA, Long-Term Care Workforce Issues: Practice Principles for Quality Dementia Care, The Gerontologist. 2018 ;58(1):S103–S113.
[11] https://ift.tt/dKcS0mo
[12] https://ift.tt/iDSaO4u
[13] https://ift.tt/NHx4eP1
[14] https://ift.tt/FqhNpj7
[15] https://ift.tt/iVcYe1R
[16] https://ift.tt/oXbuUVR
Author: Dai Tianyi
Edit: odette
Source of the title map: Figure Worm Creative
This article is from Nutshell and may not be reproduced without authorization.
If necessary, please contact [email protected]

This article is reproduced from: http://www.guokr.com/article/462265/
This site is for inclusion only, and the copyright belongs to the original author.
